Abstract
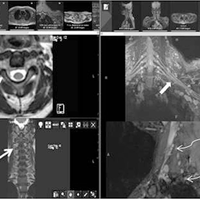
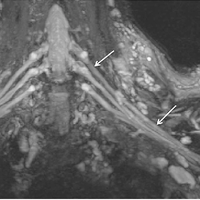
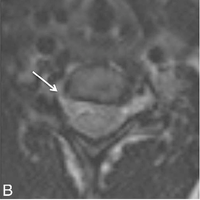
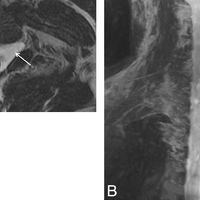
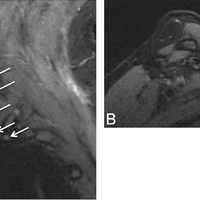
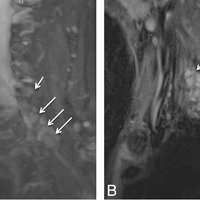
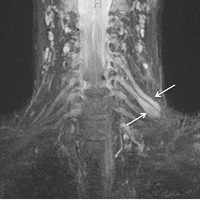
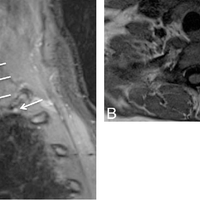
With advancement in 3D imaging, better fat-suppression techniques, and superior coil designs for MR imaging and the increasing availability and use of 3T magnets, the visualization of the complexity of the brachial plexus has become facile. The relevant imaging findings are described for normal and pathologic conditions of the brachial plexus. These radiologic findings are supported by clinical and/or EMG/surgical data, and corresponding high-resolution MR neurography images are illustrated. Because the brachial plexus can be affected by a plethora of pathologies, resulting in often serious and disabling complications, a better radiologic insight has great potential in aiding physicians in rendering superior services to patients.
Figures
Register to see more suggestions
Mendeley helps you to discover research relevant for your work.
Cite
CITATION STYLE
Chhabra, A., Thawait, G. K., Soldatos, T., Thakkar, R. S., Del Grande, F., Chalian, M., & Carrino, J. A. (2013, March). High-resolution 3T MR neurography of the brachial plexus and its branches, with emphasis on 3D imaging. American Journal of Neuroradiology. https://doi.org/10.3174/ajnr.A3287